Unseen Dangers: How Dental Infections Impact Your Overall Health

Dental infections may seem confined to the mouth, but their influence can ripple through the body in unexpected ways. At Lowry Endodontics in Denver, Colorado, we’re committed to helping patients across the Rocky Mountain region understand and address these hidden threats to their well-being. If terms like “dental infection systemic effects” or “tooth abscess complications” have brought you here, you’re wise to investigate—the links to heart, brain, sinus, artificial joints, and even pregnancy complications are well-documented and worth understanding.
Bacteria from a tooth abscess or untreated decay can travel via the bloodstream or adjacent tissues, setting off inflammatory responses elsewhere. This isn’t mere speculation; extensive research ties oral infections to heightened risks across multiple systems. For instance, in the heart, chronic dental infections have been associated with acute myocardial infarction and coronary heart disease, as bacteria contribute to arterial inflammation and plaque formation [0][1]. Epidemiological studies further suggest that periodontal disease elevates cardiovascular risks, potentially exacerbating conditions like endocarditis [7]. Similarly, for those with diabetes, oral inflammation can worsen blood sugar control, creating a vicious cycle.
The brain faces rare but severe threats from dental sources, where infections can lead to abscesses—potentially life-threatening collections of pus. Cases often arise in otherwise healthy individuals without obvious prior dental issues, with bacteria migrating upward to cause neurological symptoms [10][13]. Undetected chronic oral infections have been implicated in bacterial colonization of the brain, especially in immunocompromised patients, highlighting the need for vigilance even in “silent” cases [17].
Sinus problems represent another common pathway, with odontogenic sinusitis stemming from maxillary tooth infections invading the nearby sinuses. This can manifest as persistent sinusitis, often unilateral, triggered by dental procedures or untreated decay [30][32]. Bacterial spread from the tooth root to the sinus cavity leads to inflammation, congestion, and sometimes fungal complications, affecting breathing and quality of life [33].
For patients with artificial joints, such as hip or knee replacements, dental infections pose a particular concern due to the risk of prosthetic joint infections (PJIs). Transient bacteremia from oral sources can seed these sites, though the direct link post-dental procedures is debated; studies show varying associations, with some indicating no increased risk but emphasizing the importance of oral hygiene to mitigate potential complications [20][21][24]. These infections can be challenging to treat, often requiring antibiotics or revision surgery.
Pregnancy introduces another layer of risk, where maternal dental infections have been linked to adverse outcomes. Research indicates that periodontal disease and untreated tooth abscesses may increase the likelihood of preterm birth, low birth weight, and preeclampsia due to systemic inflammation and bacterial spread affecting placental health [25][26][27]. Pregnant patients experiencing oral symptoms should seek prompt evaluation to protect both maternal and fetal well-being.
Consider a patient who presented with unexplained headaches and fatigue. After several medical and surgical interventions, we were able to later trace this to a dental abscess that had perforated her sinus. The dental infection has causing her chronic sinus infection. Additionally, she had an unexplained high c-RP blood test indicating high inflammation throughout her body. Our high-resolution CBCT imaging pinpointed the source, and through laser-assisted irrigation (SWEEPS) and multi-visit antimicrobial therapy, we resolved the infection and healed her sinus membrane. Her c-RP blood test normalized shortly after. Follow-up at 1 year confirmed healing, underscoring how targeted endodontic care can interrupt these cascades.
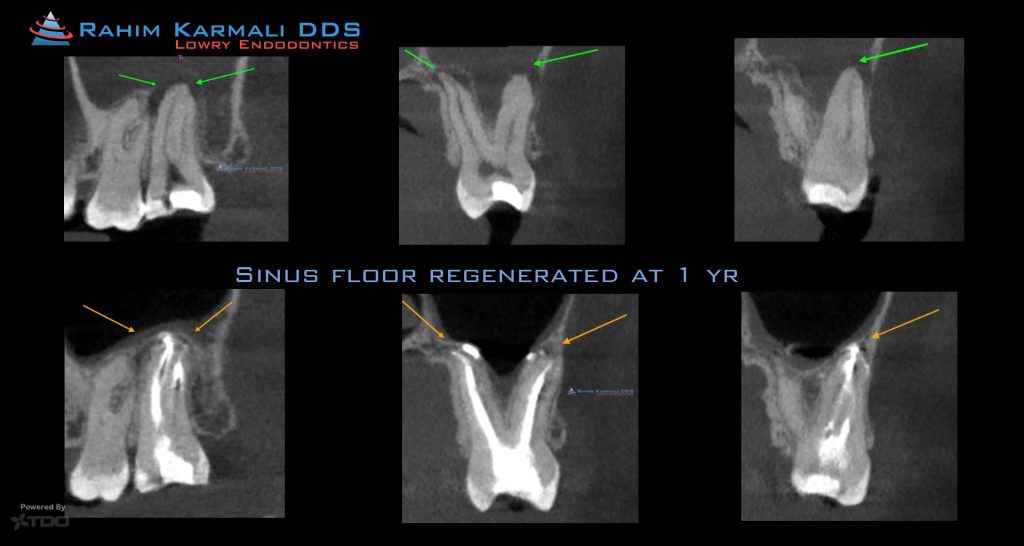
For Dr. Karmali, precision is key: CBCT scans map the infection, laser assisted irrigation (SWEEPS) ensures deep disinfection, and our protocols include antimicrobial placement between visits for thorough eradication. This contrasts with extraction routes, where implants might invite similar risks like peri-implantitis.
If symptoms like swelling, pain, or unexplained health dips suggest a dental link, especially concerning heart, brain, sinus, joints, or pregnancy, seek specialist input. We’re equipped to serve Denver, and beyond the Rocky Mountain region, with expert endodontic care. Explore www.lowryendo.com for insights, patient narratives, or to consult Dr. Rahim Karmali. Your mouth’s health is a gateway to your body’s—act on it.
[0] Li X, Kolltveit KM, Tronstad L, Olsen I. Systemic diseases caused by oral infection. Clin Microbiol Rev. 2000 Oct;13(4):547-58.
[1] Beck JD, Offenbacher S, Williams R, et al. Periodontitis: a risk factor for coronary heart disease? Ann Periodontol. 1998;3(1):127-41.
[7] Lockhart PB, Bolger AF, Papapanou PN, et al. Periodontal disease and atherosclerotic vascular disease: does the evidence support an independent association? A scientific statement from the American Heart Association. Circulation. 2012;125(20):2520-44.
[10] Corson MA, Postlethwaite KP, Seymour RA. Are dental infections a cause of brain abscess? Case report and review of the literature. Oral Dis. 2001;7(3):61-5.
[13] Gendron R, Grenier D, Maheu-Robert LF. The oral cavity as a reservoir of bacterial pathogens for focal infections. Microbes Infect. 2000;2(8):897-906.
[17] Tonetti MS, Van Dyke TE; Working group 1 of the joint EFP/AAP workshop. Periodontitis and atherosclerotic cardiovascular disease: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Clin Periodontol. 2013;40 Suppl 14:S24-9.
[20] Keene JJ, Galasko G, Landis GH, et al. Antimicrobial prophylaxis in prosthetic joint infections: a review of evidence and guidelines. J Am Dent Assoc. 2003;134(7):1041-8.
[21] Watters W 3rd, Rethman MP, Hanson NB, et al. Prevention of orthopaedic implant infection in patients undergoing dental procedures. J Am Acad Orthop Surg. 2013;21(3):180-9.
[24] Berbari EF, Osmon DR, Carr A, et al. Dental procedures as risk factors for prosthetic hip or knee infection: a hospital-based prospective case-control study. Clin Infect Dis. 2010;50(1):8-14.
[25] Offenbacher S, Lieff S, Boggess KA, et al. Maternal periodontitis and prematurity. Part I: Obstetric outcome of prematurity and growth restriction. Ann Periodontol. 2001;6(1):42-9.
[26] Xiong X, Buekens P, Fraser WD, et al. Periodontal disease and adverse pregnancy outcomes: a systematic review. BJOG. 2006;113(2):135-43.
[27] Boggess KA, Lieff S, Murtha AP, et al. Maternal periodontal disease is associated with an increased risk for preeclampsia. Obstet Gynecol. 2003;101(2):227-31.
[30] Mehra P, Jeong D. Maxillary sinusitis of odontogenic origin. Curr Allergy Asthma Rep. 2009;9(3):205-10.
[32] Abrahams JJ, Glassberg RM. Dental disease: a frequently unrecognized cause of maxillary sinus abnormalities? AJR Am J Roentgenol. 1996;166(5):1219-23.
[33] Brook I. Sinusitis of odontogenic origin. Otolaryngol Head Neck Surg. 2006;135(3):349-55.
